Many digestive diseases have similar
symptoms. Here’s how to recognize them and when to visit your doctor. Most
people don’t like to talk about it, but having a gastrointestinal problem is
common. There’s no need to suffer in silence. Here’s a top-to-bottom look at
most prevalent digestive conditions, their symptoms, and the most effective
treatments available. If you suspect you could have one of these issues, don't
delay in speaking with your doctor. Top of Form Bottom of Form abdominal pain
is a common symptom for several different digestive conditions, so it’s
important to visit your doctor to get an accurate diagnosis. Twenty million
Americans are affected by gallstones. Obesity is a risk factor for multiple
digestive problems, including hemorrhoids and diverticulitis. Most people don’t
like to talk about it, but having a gastrointestinal problem is common. There’s
no need to suffer in silence. Here’s a top-to-bottom look at nine of the most
prevalent digestive conditions, their symptoms, and the most effective
treatments available. If you suspect you could have one of these issues, don't
delay in speaking with your doctor.
Chest Pain:
Gastroesophageal Reflux Disease (GERD)

When stomach acid backs up into your
esophagus, a condition called acid reflux, you may feel a burning pain in the
middle of chest. It often occurs after meals or at night, says Necille Bamji,
MD, a clinical instructor of medicine at The Mount Sinai Hospital and a
gastroenterologist with New York Gastroenterology Associates. While it’s common
for people to experience acid reflux and heartburn once in a while, having
symptoms that affect your daily life or occur at least twice each week could be
a sign of GERD, a Chronic digestive disease that effects 20 percent of
Americans, according to the National Institute of Diabetes and Digestive and
Kidney Diseases (NIDDK). If you experience persistent heartburn, bad breath,
tooth erosion, nausea, pain in your chest or upper part of your abdomen, or
have trouble swallowing or breathing, see your doctor. Most people find relief
by avoiding the foods and beverages that trigger their symptoms and/or by
taking over-the-counter antacids or other medications that reduce stomach acid
production and inflammation of the esophagus; however, some cases of
GERD require stronger treatment, such as medication or surgery.
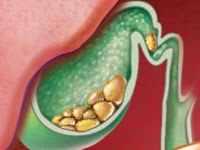
Gallstones
Gallstones are hard deposits that
form in your gallbladder, a small, pear-shaped sack that stores and secretes
bile for digestion. Twenty million Americans are affected by gallstones,
according to the NIDDK. Gallstones can form when there’s too much Cholesterol
or waste in your bile or if your gallbladder doesn’t empty properly. When
gallstones block the ducts leading from your gallbladder to your intestines,
they can cause sharp pain in upper right abdomen. Medications sometimes
dissolve gallstones, but if that doesn’t work, the next step is surgery to
remove the gallbladder.
Celiac Disease

An estimated 1 in 133 Americans has
celiac disease, according to the National Foundation for Celiac Awareness, but
it’s also estimated that 83 percent of people who have celiac disease don’t
know they have it or have been misdiagnosed with a different condition. Celiac
disease is a serious sensitivity to gluten, a protein found in wheat, rye, and
barley. Eat gluten, and your immune system goes on the attack: It damages your
villi, the fingerlike protrusions in your small intestines that help you absorb
nutrients from the foods you eat. Symptoms of celiac disease in kids include
abdominal pain and bloating, diarrhea, constipation, vomiting, and weight loss.
Symptoms in adults also can include anemia, fatigue, bone loss, depression, and
seizures. However, some people may not have any symptoms. The only treatment
for celiac disease is to completely avoid eating gluten. Common cooking
alternatives to gluten include brown rice, quinoa, lentils, soy flour, corn
flour, and amaranth.
Crohn’s Disease
Crohn’s disease is part of a group
of digestive conditions called inflammatory bowel disease (IBD). Crohn’s most
commonly affects the end of the small intestine called the ileum, but it can
affect any part of the digestive tract. As many as 700,000 Americans may be
affected by Crohn’s, according to the Crohn’s and Colitis Foundation of
America. This chronic condition is an autoimmune disease, meaning that your
immune system mistakenly attacks cells in your own body that it thinks are
foreign invaders. The most common Crohn’s symptoms are abdominal pain,
diarrhea, rectal bleeding, weight loss, and fever. “Treatment depends on the
symptoms and can include topical pain relievers, immunosuppressants, and
surgery,” Dr. Bamji says.
Ulcerative Colitis
Ulcerative colitis is another
inflammatory bowel disease that affects about 700,000 Americans. The symptoms
of ulcerative colitis are very similar to those of Crohn's, but the part of the
digestive tract affected is solely the large intestine, also known as the
colon. If your immune system mistakes food or other materials for invaders,
sores or ulcers develop in the colon’s lining. If you experience frequent and
urgent bowel movements, pain with diarrhea, blood in your stool, or abdominal
cramps, visit your doctor. Medication can suppress the inflammation, and
eliminating foods that cause discomfort may help as well. In severe cases, treatment
for ulcerative colitis may involve surgery to remove the colon.
Irritable Bowel
Syndrome

Is your digestive tract irritable?
Do you have stomach pain or discomfort at least three times a month for several
months? It could be irritable bowel syndrome (IBS), another common digestive
condition. Ten to 15 percent of the U.S. population suffers from irritable
bowel syndrome, according to the International Foundation for Functional
Gastrointestinal Disorders. Signs of IBS can vary widely: You can be
constipated or have diarrhea, or have hard, dry stools on one day and loose
watery stools on another. Bloating is also a symptom of IBS. What causes IBS
isn’t known, but treatment of symptoms centers largely on diet, such as
avoiding common trigger foods (dairy products, alcohol, caffeine, artificial
sweeteners and beans, cabbage, and other foods that produce gas), or following
a low-fat diet that's also high in fiber. Friendly bacteria, such as the pro-biotic
found in live yogurt, may also help you feel better. Stress can trigger IBS symptoms,
so some people find cognitive-behavioral therapy or low-dose antidepressants to
be useful treatments, as well.
Hemorrhoids
Bright red blood in the toilet bowl
when you move your bowels could be a sign of hemorrhoids, which is a very
common condition. In fact, 75 percent of Americans over the age of 45 have
hemorrhoids, according to the NIDDK. Hemorrhoids are an inflammation of the
blood vessels at the end of your digestive tract. They can be painful and
itchy. Causes include chronic constipation, diarrhea, straining during bowel
movements, and a lack of fiber in your diet. Treat hemorrhoids by eating more
fiber, drinking more water, and exercising. Over-the-counter creams and
suppositories may provide temporary relief of hemorrhoid symptoms. See your
doctor if at-home treatments don’t help; sometimes a hemorrhoidectomy is
needed to remove hemorrhoids surgically.
Diverticulitis
Small pouches called diverticula can
form anywhere there are weak spots in the lining of your digestive system, but
they are most commonly found in the colon. If you have diverticula but no symptoms,
the condition is called diverticulosis, which is quite common among older
adults and rarely causes problems; however, if the pouches bleed or become
inflamed, it’s called diverticulitis. Symptoms include rectal bleeding, fever,
and abdominal pain. Obesity is a major risk factor for diverticulitis. Mild diverticulitis
is treated with antibiotics and a liquid diet so your colon can heal. A low
fiber diet could be the cause of diverticulitis, so your doctor may direct you
to eat a diet high in fiber — whole grains, legumes, vegetables — as part of
your treatment. If you have severe attacks that recur frequently, you may need
surgery to remove the diseased part of your colon.
Anal Fissure
Anal fissures are tiny, oval-shaped
tears in the lining of the very end of your digestive tract called your anus.
The symptoms are similar to those of hemorrhoids, such as bleeding and pain
after moving your bowels. Straining and hard bowel movements can cause
fissures, but so can soft stools and diarrhea. A high-fiber diet that makes
your stool well formed and bulky is often the best treatment for this common
digestive condition. Medications to relax the anal sphincter muscles as well as
topical anesthetics and sitz baths can relieve pain; however, chronic fissures
may require surgery of the anal sphincter muscle.
in the next post we will discuss about Causes, Symptoms, Test and Treatment of Hepatitus C Virus